COVID-19: Implications for the Water and Wastewater Industry
April 1, 2020
John Bergendahl, Ph.D., P.E., Associate Professor, Dept. of Civil and Environmental Engineering, Worcester Polytechnic Institute, Worcester MA, jberg@wpi.edu
Marina Fernandes, P.E., LEED AP, Tighe & Bond, Westwood MA
Wayne E. Bates, Ph.D., P.E., Tighe & Bond, Westwood MA
INTRODUCTION
In December 2019, multiple cases of respiratory illness in Wuhan, China started being reported. Initially the origin of these pneumonia cases could not be identified, but before long a novel severe acute respiratory syndrome (SARS) virus, SARS-CoV-2, was identified as the cause of the coronavirus disease of 2019, COVID-19. Symptoms include dry cough, fever, and respiratory distress. Its initial transmission to people was narrowed to a seafood and animal market in Wuhan, but it has been suggested that SARS-CoV-2 likely originated in bats (Chan et al., 2020). It was soon determined that person-to-person transmission was occurring, and before long a large number of people in the area became ill. As of April 1, 2020, more than 820,000 people world-wide have contracted COVID-19 with over 40,000 deaths reported (WHO, novel-coronavirus-2019). Only through drastic measures, including shuttering businesses and quarantining residents, was the outbreak mitigated in China. However, by that time, COVID-19 had started spreading around the world, resulting in the World Health Organization (WHO) declaring a pandemic in early March.
SARS-CoV-2 is a newly-discovered strain of coronavirus, related to other serious strains including Severe Acute Respiratory Syndrome (SARS-CoV) and Middle East Respiratory Syndrome (MERS-CoV). In addition, there are many other coronaviruses that are much less serious to human health, and many that are currently known to infect animals. Both SARS-CoV and MERS-CoV resulted in deadly outbreaks; the SARS outbreak in 2003 infected 8,096 people with 9.6% fatality rate, and MERS has infected 2,494 people since 2012 with a 34.4% fatality rate (data from the World Health Organization).
As the details on the COVID-19 pandemic are still emerging, those in the water and wastewater industry have many questions:
Can we be exposed to SARS-CoV-2 virus through direct, or indirect, contact with wastewater or wastewater droplets? 1
Can the SARS-CoV-2 be released to the environment through treatment facility discharges? 2
As SARS-CoV-2 is zoonotic, can the virus be passed to animals who contact it after wastewater discharge? 2
Can the SARS-CoV-2 virus persist in water sources and be taken into drinking water facilities? 2
What are the roles that water/wastewater professionals will play going forward in preparing for future pandemics? Should our approach to infrastructure strive to become more resilient to disruptions from pandemics? 3
- With proper disinfection, this is not likely. Infection is possible from sewage that is not disinfected.
- Low likelihood, but needs research.
- Very important that the industry addresses our role in preventing pandemics and providing resilience.
TRANSMISSION, INCLUDING FROM WASTEWATER
The SARS-CoV-2 coronavirus, which causes the COVID-19 disease, has been found to have similarities to the 2003 strain of coronavirus that was responsible for the deadly 2003 outbreak, SARS-CoV. Research has shown that the SARS-CoV-2 genome is 82% similar to the SARS-CoV genome (Chan et al., 2020), and the disease progression is comparable. Both have an incubation (mean) time of five days, identical risk factors (age, and effect of underlying illnesses), and can result in development of respiratory distress within 8 – 20 days after the first symptoms initiate (Wilder-Smith et al., 2020). However the spread of SARS-CoV and SARS-CoV-2 through the community has been dramatically different … while SARS-CoV was effectively controlled with applied public health measures (control of public events, quarantines, temperature monitoring, personal protective equipment for hospital personnel, etc.), the spread of SARS-CoV-2 has continued worldwide resulting in a pandemic. Greater population densities and more global travel has certainly contributed to the rapid spread of SARS-CoV-2 compared to SARS-CoV. But the apparent high degree of transmissibility is a likely factor to its wide and rapid spread. And it has been found that the transmission of this virus occurs earlier after initial infection, even before symptoms are obvious (Wilder-Smith et al., 2020). Contributing to its transmission is the fact that this virus has a wide range of symptoms, from asymptomatic, to mild, to severe – yet patients within the range of symptoms can be infectious. Clearly the effectiveness and complexity of this novel coronavirus contribute to its persistence and transmissivity, and are primary reasons for the resulting pandemic.
As the main symptoms of COVID-19 infection are respiratory (Zhu et al., 2020), it should be expected that the virus may be shed and transmitted through the respiratory route even when no symptoms are exhibited. Transmission is thought to be through exposure to aerosol/droplets of respiratory origin, and through contact with contaminated surfaces. The shedding and movement of the virus through these mechanisms thus requires protective protocols to prevent spread via these routes. Recent research has found that the SARS-CoV-2 virus remains viable in aerosols for hours, and can persist as viable on many surfaces for days (van Doremalen et al., 2020).
In addition, recent findings indicate that the virus is also shed in the feces of infected people suggesting a possible additional route of transmission via the gastrointestinal system (Gu et al., 2020). Xie et al. (2020) found positive nucleic acid test results for the SARS-CoV-2 virus in the feces of eight of nineteen infected patients. In comparison, nine of these patients had positive throat swabs – which is currently considered the appropriate novel coronavirus test. However, no cases of COVID-19 through the transmission of SARS-CoV-2 virus via untreated wastewater or defective plumbing have been recorded. The presence of SARS-CoV-2 virus in feces gives concern due to the possible effect on public health via water-borne (water, wastewater, contaminated surface water) virus mobility. This issue is exacerbated by the significant number of COVID-19 patients who exhibit diarrhea (Xie et al., 2020). In one report by Wang et al. (2020), 10% of COVID-19 infected patients in China had diarrhea. As diarrhea had been reported to be as high as 27% for SARS-CoV (Donnelly et al., 2003; He et al., 2020), it may be expected to be higher for COVID-19 than currently reported. In addition, it was found that infected individuals can shed virus in their feces for a much longer time period than the time period that respiratory samples were positive (Ma et al., 2020).
PRESENCE IN WASTEWATER, WITH CONSIDERATION FOR RESIDENTIAL PLUMBING SYSTEMS
Disinfection is one of the primary approaches that water and wastewater professionals have for controlling pathogens in water and wastewater. As SARS-CoV-2 has a similar genome to SARS-CoV, it should be anticipated to behave similarly. Research by Wang et al. (2005b) found that SARS-CoV in wastewater was susceptible to sodium hypochlorite and chlorine dioxide, with effective inactivation at reasonable dosages and contact times. In fact, Wang et al. reported that SARS-CoV was inactivated at lower dosages and contact times than required for E. coli and f2 phage. Unfortunately the persistence of SARS-CoV without disinfection was troubling – Wang et al. (2005b) found that SARS-CoV persisted for up to 14 days in wastewater and 17 days in feces and urine at 4oC.
As the genome is very similar to SARS-CoV, experiences with the 2003 SARS outbreak are illuminating. In one cluster of infections in a housing complex (the Amoy Gardens) during the 2003 SARS epidemic in Hong Kong, the primary route of transmission for the cluster was determined to be through a defective sewage system in the building (Lee, 2003). It was determined that a significant viral load was released into the building sewage system from infected individuals who were suffering from diarrhea. The virus was then drawn from the sewage system into the drains in other bathrooms in droplet form, where it deposited on various surfaces in the living spaces. From this mechanism of infection via sewage droplets, the virus infected 321 people in this housing block. This transmission was thought to have occurred due to the water traps in the drains becoming empty of water – proper operation/maintenance of the U-shaped water traps is for water to be maintained in the trap to prohibit passage of noxious gasses, insects, etc. The findings from the study of this cluster suggest that coronaviruses of the SARS type may be present in domestic wastewater, and depending on the wastewater collection system dynamics, may provide for an infectious situation. Further evidence of the potential for infection via sewage was reported by Wang et al. (2005a) where SARS-CoV nucleic acid was identified in sewage from Hong Kong hospitals treating SARS patients.
More recently, according to a February 12, 2020 CNN report, a Hong Kong building was partially evacuated and some residents quarantined, after two cases of COVID-19 were suspected to be connected as the result of faulty sewage piping. In this case reported by CNN, a 62 year old female resident contracted COVID-19 approximately 10 days after a 75 year old male resident had tested positive for COVID-19. While not confirmed as of the date of this publication, it is suspected that a detached sewer vent pipe in the woman’s apartment may have been a possible transmission route for aerosolized sewage that may have contained coronavirus.
The confirmed 2003 cases in Hong Kong, and the unconfirmed 2020 case also in Hong Kong, illustrate the potential exposure risks associated with aerosolized sewage droplets. While to date there are no confirmed cases of COVID-19 from contact with raw sewage, the transmission of SARS-CoV-2 is not yet fully understood, which makes it more important than ever to continue proactive sewer system operation and maintenance to help reduce the potential exposure to raw sewage, especially in the aerosol form. Protecting the general public from exposure to raw sewage is a fundamental objective of every sewer authority and is accomplished through a variety of proactive maintenance measures such as cleaning and inspecting, inflow and infiltration investigations, illicit discharge elimination programs, pump station inspections, as well as other routine and capital improvement activities. It is equally important for sewer authorities to educate the general public on their role in maintaining a functional sewer system by not flushing “disposable” disinfecting wipes or paper towels. The public must understand that these products do not break down like toilet paper and excessive amounts have led to sewer main blockages, residential backups, and pump station damage. The general public should also be aware that sewer blockages can increase the potential exposure to raw sewage when sewage backs up into residential dwellings or raw sewage overflows to surface waters.
BIOSOLIDS / DISPOSAL HANDLING
The persistence of the coronavirus in wastewater also gives concern for the release and transmission of the virus through biosolids handling and disposal operations. Until further investigations are performed, it is reasonable to assume that unstabilized primary and secondary sludges generated by wastewater treatment operations will have similar exposure risk and virus viability durations as raw wastewater. Exposure potential occurs during processing operations at wastewater treatment facilities, as well as at disposal sites receiving unstabilized sludges. Biosolids which are land applied typically undergo advanced stabilization processes (anaerobic digestion, thermal drying, lime stabilization, composting, etc.) to reduce pathogens, as regulated by 40 CFR Part 503 (Standards for the Use or Disposal of Sewage Sludge). While these stabilization processes are well-developed, some published research illustrates that there still may be viral pathogens present after applying these techniques. In one study by Wong et al. (2010), various enteric viruses were found in biosolids after mesophilic anaerobic digestion (including norovirus and human adenoviruses). Further, the possibility of runoff from biosolids-amended agricultural land containing viral contamination was illustrated by Wong et al. (2012). Additional research is recommended to confirm SARS-CoV-2 is no longer viable following biosolids stabilization processes.
DOMESTIC WASTEWATER REUSE
Domestic wastewater reuse applications must consider the risk of possible contamination by the coronavirus. Exposure should be considered from both direct contact as well as aerosols if the water is not properly disinfected. Water reuse projects typically employ multiple disinfection barriers that are known to be effective for a range of bacteria and viruses including SARS-CoV and MERS-CoV. Typical disinfection processes include chlorination, ozonation, and UV disinfection. Regulations such as California Title 22 require extended chlorine contact time or disinfection processes that provide at least 99.999% (i.e., 5-log) removal or inactivation of MS2 (a surrogate virus) or polio virus for tertiary recycled water. Direct and indirect potable reuse applications typically have more advanced disinfection requirements. For example, California Title 22 regulations require indirect potable reuse projects such as groundwater replenishment reuse projects to provide up to 12-log enteric virus reduction. Additional research is recommended to confirm SARS-CoV-2 is no longer viable following typical water reuse disinfection processes.
PROACTIVE COLLECTION SYSTEM OPERATIONS
Proactive measures such as the development of capacity, management, operation, and maintenance (CMOM) programs are even more critical in the time of COVID-19 to help reduce the overall potential for society to encounter wastewater. Not only are regulators throughout New England emphasizing a need for enhanced CMOM programs through permit requirements and state regulations, communities are becoming more strategic with local budgets by undertaking an asset management approach to utility operations, resulting in staff and contractors encountering wastewater even more frequently than a decade ago. These entities are completing proactive routine system maintenance, such as jetting, manhole repairs, and pump station visits, studies (such as infiltration and inflow metering and inspections), and capital improvements including collection rehabilitation or replacement, and pump station and treatment plant repairs and upgrades.
In addition to the physical maintenance activities, system operators are also investing in public education on the challenges facing the industry from aging assets to operational challenges related to societal issues such as non-flushable wipes. In a March 30, 2020 release, the federal EPA encourages Americans to only flush toilet paper and states that “Preventable toilet and sewer backups can pose a threat to human health and present an extra challenge to our water utilities and their workforce. Flushing anything other than toilet paper, including disinfecting wipes, can damage internal plumbing, local sewer systems and septic systems. Fixing these backups is costly and takes time and resources away from ensuring that wastewater management systems are otherwise working properly” (EPA, 03/30/2020). This is a message that system operators must continue to convey to its customer base.
Each of these efforts play a part in keeping the system functional, reducing the potential for sanitary sewer overflows into a private homes or businesses, the streets, or local waterbodies, and thereby limiting the potential for the public to come into contact with COVID-19 in wastewater.
HEALTH AND SAFETY IN THE WASTEWATER INDUSTRY
The presence of novel coronavirus in wastewater, and its possible long-term viability should come as a serious concern for practitioners in this industry. There is no doubt that we need to protect ourselves from the many other pathogens that are known to be present in wastewater, but the high infectivity and possible severe health consequences of COVID-19 requires that we take extra precautions. And we should expect an increased SARS-CoV-2 viral load in wastewater as more of the population becomes infected as projected. Protection from raw sewage, and aerosol droplets that may drift from the sewage, is necessary. Deposition of SARS-CoV-2 on surfaces exposed to droplets should be expected. Generally, handling of waste that is suspected or known to contain COVID-19 does not require special precautions or personal protection equipment (PPE) beyond those already used to protect workers from the hazards they encounter during their routine job tasks in solid waste and wastewater management.
CONCERNS IN THE DEVELOPING WORLD
In addition to the concerns of the coronavirus pandemic in the United States, the impact may be critical in the developing world. The ability to test for the presence of coronavirus in sick patients, and an adequate health care system with the availability of trained health professionals, may be compromised in other countries. Both WHO and CDC are suggesting that people wash their hands frequently to help prevent the spread of the novel coronavirus (or use an alcohol-based hand sanitizer) … yet many in the developing world do not have adequate access to clean water and sanitation facilities to do this. As of 2017, 2.2 billion people did not have access to safely-managed water, 4.2 billion people do not have acceptable sanitation, and 3 billion people do not have access to simple handwashing facilities (according to the WHO). In many undeveloped areas of the world, there may be direct fecal contamination of surface waters used for drinking, washing, and other domestic activities. As an example, there is an ongoing shortage of potable water in Rio de Janeiro that has extended since February, due to concerns about possible contamination of the city’s water supply; CEDAE, the state-owned water utility, was forced to temporarily shut down a key treatment plant, resulting in water shortages in dozens of neighborhoods. Today, these same neighborhoods are forced to go without water for much of the day, impeding them of properly washing their hands and sanitizing their homes amidst the pandemic. There are many examples such as this in the developing world where lack of proper sanitation facilities can lead to illnesses.
Our industry should take a strengthened initiative to alleviate these shortcomings throughout the world as pandemics such as coronavirus may be controlled with increased access to clean water and sanitation around the world. The world may have been unprepared for the arrival of COVID-19, and its increased infection rate/death toll due to poor sanitation in the developing world is still unknown as the peak has not arrived in those countries yet. However, in the near future, discussions in regards to increased sanitation investments will be necessary as we prepare for future outbreaks in parts of the world where sanitation is lacking.
CONCLUSIONS
Recent findings on the novel coronavirus SARS-CoV-2 infectivity, high degree of shedding from the human body, and persistence in the environment, coupled with our knowledge of the 2003 SARS-CoV epidemic, provides some insight into the impacts on the water and wastewater industry. In the 2003 SARS epidemic, a significant number of individuals were found to have been infected through sewage, with the route of transmission via droplets. As the SARS-CoV-2 virus, which causes the COVID-19 infection, is similar to the SARS-CoV virus, the water and wastewater industry must be cognizant of the potential for water-borne or sewage-borne routes for infection. While the SARS-CoV-2 virus is thought to be readily inactivated through disinfection processes typical for the industry, extra precautions are probably prudent to prevent infecting personnel in the industry and the public. In addition, it is crucial to prevent discharge of the virus to the environment, and prevent contamination of drinking water sources and systems. Research is needed to determine the persistence of the SARS-CoV-2 virus in water systems, wastewater systems, and the environment, and to determine the best engineering actions going forward to control the pandemic.
For additional information:
https://www.who.int/health-topics/coronavirus
https://www.cdc.gov/coronavirus/2019-ncov/php/water.html
https://www.wef.org/news-hub/wef-news/the-water-professionals-guide-to-the-2019-novel-coronavirus/
https://www.osha.gov/SLTC/covid-19/controlprevention.html).
https://www.newea.org/covid-19-updates/
References
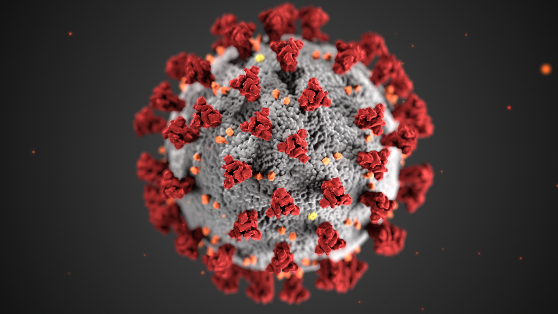
CDC; Centers for Disease Control and Prevention, SARS-CoV-2 figure by Alissa Eckert and Dan Higgins, 2020.
Chan, J., Kok, K., Zhu, Z., Chu, H., To, K., Yuan, S., and Yuen, K.; “Genomic Characterization of the 2019 Novel Human-Pathogenic Coronavirus Isolated from a Patient with Atypical Pneumonia After Visiting Wuhan”, Emerging Microbes & Infections, 9, 221-236, 2020.
Donnelly, C., et al.; “Epidemiological Determinants of Spread of Causal Agent of Severe Acute Respiratory Syndrome in Hong Kong”, The Lancet, 361, 1761-1766, 2003.
EPA, “EPA Encourages Americans to Only Flush Toilet Paper”, News Releases from Headquarters, March 30, 2020.
Gu, J., Han, B., and Wang, J.; “Gastrointestinal Manifestations and Potential Fecal-Oral Transmission”, Gastroenterology, pre-proof accepted February 26, 2020.
He, Y., Wang, Z., Li, F., and Shi, Y.; “Public Health Might be Endangered by Possible Prolonged Discharge of SARS-CoV-2 in Stool”, Journal of Infection, accepted February 28, 2020, in press.
Lee, S.H.; “The SARS Epidemic in Hong Kong”, Journal of Epidemiology and Community Health, 57, 652, 2003.
Ma, X., Su, L., Zhang, Y., Zhang, X., Gai, Z., Zhang, Z.; “Do Children Need a Longer Time to Shed SARS-CoV-2 in Stool Than Adults”, Journal of Microbiology, Immunology and Infection, pre-proof, https://doi.org/10.1016/j.jmii.2020.03.010
Van Doremalen, N., Bushmaker, T., et al.; “Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1”, N Engl J Med, published March 17, 2020 at NEJM.org.
Wang, D., Hu, B., et al.; “Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China”, JAMA, 323(11), 1061-1069, 2020.
Wang, X., Li, J., et al.; “Concentration and Detection of SARS Coronavirus in Sewage from Xiao Tang Shan Hospital and the 309th Hospital”, Journal of Virological Methods, 128, 156-162, 2005(a).
Wang, X., Li, J., et al.; “Study on the Resistance of Severe Acute Respiratory Syndrome-Associated Coronovirus”, Journal of Virological Methods, 126, 171-177, 2005(b).
WHO; World Health Organization, https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
Wong, K., Onan, B.M., and Xagoraraki, I.; “Quantification of Enteric Viruses, Pathogen Indicators, and Salmonella Bacteria in Class B Anaerobically Digested Biosolids by Culture and Molecular Methods”, Applied and Environmental Microbiology, 76 (19), 6441-6448, 2010.
Wong, K., Harrigan, T., and Xagoraraki, I.; “Leaching and Ponding of Viral Contaminants Following Land Application of Biosolids on Sandy-Loam Soil”, Journal of Environmental Management, 112, 79-86, 2012.
Xie, C., Jiang, L., et al.; “Comparison of Different Samples for 2019 Novel Coronavirus Detection by Nucleic Acid Amplification Tests”, International Journal of Infectious Diseases, 93, 264-267, 2020.
Wilder-Smith, A., Chiew, C.J., and Lee, V.J.; “Can We Contain the COVID-19 Outbreak with the Same Measures as for SARS”, Lancet Infect Dis, March 5, 2020.
Zhu, N., Zhang, D., et al.; “A Novel Coronavirus from Patients with Pneumonia in China, 2019”, N Engl J Med, 382, 727-733, 2020.



No comments yet.